Jayme Spangler, a biller at Hershey Pediatrics in Hershey, Pennsylvania, said that since becoming a Level 3 PCMH in 2014, the office has been much more efficient. “We’re more on task now with things that used to fall through the cracks. We have better follow-up with patients and our workflow has improved.”
Dr. George Rogu, a managing provider at RBK Pediatrics in Commack, New York, said of the process: “It is a rigorous internal evaluation and restructuring of the culture, process and procedures of the practice. But the end result is a superior quality of care that will ultimately result in a reduction of health care expenditures and a positive experience for patients.”
The main question that many pediatricians are asking is: “Should I try for PCMH accreditation?” Our goal is to provide answers that will help you decide if PCMH recognition is worth your time and money.
Is My Practice Eligible?
To be eligible, your practice must do all of the following:
- Provide whole-person care
- Have a personal clinician who provides first contact, continuous, comprehensive care
- Provide care that is coordinated or integrated across the health care system
- Have team-based care
The National Committee for Quality Assurance (NCQA) offers a short guide and a video to help clarify eligibility requirements. Be sure to find out if your practice is eligible before proceeding on the path to PCMH recognition.
“PCMH attempts to satisfy a quadruple aim: provide better quality care, be more cost effective, and increase satisfaction of both the patient and the provider. It’s a rigorous process, but it’s the right thing to do for better quality medicine.”
Who Provides PCMH Recognition?
There are several national programs that award this distinction, including the Accreditation Association for Ambulatory Health Care (AAAHC), The Joint Commission (JCAHO), the National Committee for Quality Assurance (NCQA), and the Utilization Review Accreditation Commission (URAC). There are also excellent regional programs, such as the Oregon State Program, as well as private payer programs, such as the one offered by Blue Cross Blue Shield of Michigan.
What are the PCMH Standards?
NCQA PCMH recognition is currently based on the following six standards:3
1. Patient-Centered Access:
Accommodate patients’ needs during and after hours, provide medical home information, and offer team-based care
2. Team-Based Care:
Engage all team members by providing medical home information, meet cultural and linguistic needs of patients, and offer team-based care
3. Population Health Management:
Proactive management of patient data for population management
4. Care Management and Support:
Use evidence-based guidelines for preventive, acute and chronic care management
5. Care Coordination and Care Transitions:
Track and coordinate tests, referrals and care transitions
6. Performance Measurement and Quality Improvement:
Use performance and experience data for continuous improvement
What Are the Different Levels of Recognition?
NCQA offers three levels of PCMH recognition. Practices have to meet the above six standards and are given a score based on how well they meet the criteria. The table below describes the standards, points, and must-pass elements for each level.4
PCMH Scoring Summary
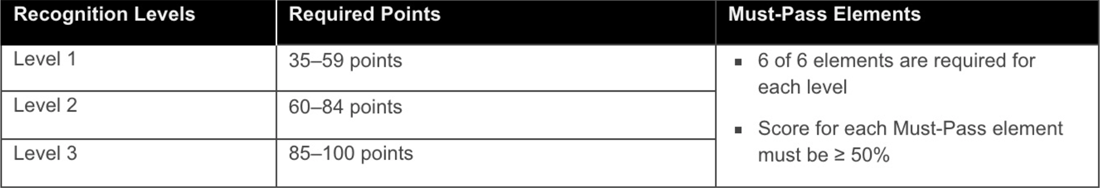
Many insurance companies only offer incentives to those practices that have Level 2 recognition or higher. To receive Level 3 recognition, you’ll need an EHR. If your practice has not yet started using an EHR for charting purposes, you may still be able to receive Level 1 or Level 2 recognition. Without EHR functionality such as electronic charting, e-prescribing, a patient portal including secure messaging, and computerized provider order entry (CPOE) for referrals and labs, you will find it very difficult if not impossible to meet the requirements for Level 3 recognition.
Before starting the recognition process, make sure to check with your software vendors, as they can be pre-validated for PCMH credits. If your vendor is pre-validated, you can automatically meet some of the factors due to functionality provided by your software. This can greatly simplify your application process.
What Are the Benefits?
There can be substantial financial incentives for PCMH recognition. Care coordination is one of many clinical initiatives your practice and patients will benefit from. Some payers offer a flat rate bonus based on visit rate while others provide bonuses based on the number of patients enrolled in their plans. These bonuses can add up quickly to make a significant difference in your bottom line. Note that these bonus amounts fluctuate based on the level of accreditation you receive.
It’s worth doing some research on the incentives offered by the payers in your area, as they vary greatly by region. Before you decide whether or not to try for PCMH recognition, you’ll want to visit the Patient-Centered Primary Care Collaborative website, which details incentives by state.
Are There Any Other Benefits?
In addition to receiving bonuses from insurance companies, becoming an accredited PCMH can give you more leverage in negotiating better fee schedules. Insurance companies offer these incentives because coordination of care ultimately saves them money.
A lesser known benefit is that PCMH-recognized practices receive credit toward Maintenance of Certification (MOC). According to the American Board of Pediatrics:
Another benefit to consider is that PCMH recognition can help you stay competitive. According to Tim Proctor, pediatric solutions consultant for PCC, “If all the practices in your area are a Level 3 PCMH, you may want to apply to help you stay marketable. Or, if a pediatrician is getting ready to sell the practice, they may want to apply to put their practice in good standing.” Going forward, it may also help in attracting new patients. “While many consumers are not yet aware what PCMH recognition means, that seems to be changing quickly,” said Proctor. If other practices in your area haven’t become recognized Patient-Centered Medical Homes, being the first or only PCMH helps set you apart from your competitors.
“We’re more on task now with things that used to fall through the cracks. We have better follow-up with patients and our workflow has improved.”
How Much Does it Cost?
The cost to apply for PCMH recognition varies by the number of providers and locations. Below is the NCQA pricing summary for single location practices:6
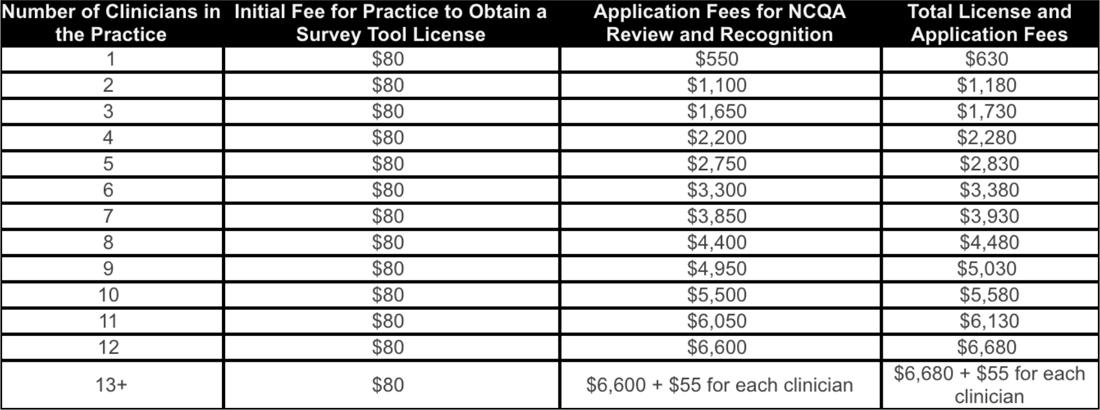
In addition to the application fees, there are a number of other costs to factor in, such as whether you will hire a consultant or additional personnel, and whether you need to upgrade any office equipment or software to meet the criteria.
For multi-location practices, not only is the process more expensive, it’s also more challenging.
“A portion of your PCMH application is site-specific,” said Proctor. “This requires you to report certain clinical measures uniquely by location. This can be challenging because many multi-location practices operate as one collective practice. For example, it can be difficult to report on immunization or well-child visit rates per location if patients visit more than one location and if you work together as a practice to care for those patients.”
How Does PCMH Help Provide Better Care?
While there are currently a number of cumbersome aspects to applying for PCMH recognition, many pediatric practices say it has forced them to improve their processes. “Many practices see improvement with things like tracking referrals, tracking tests, and following up on lab results,” said Proctor.
And, Proctor said, 2014 PCMH standards call for integrating behavioral health in your practice. “This is an improvement in terms of quality of care, as practices must now show how they’re doing care planning and management for certain behavioral conditions.”
Dr. Rogu said: “PCMH attempts to satisfy a quadruple aim: provide better quality care, be more cost effective, and increase satisfaction of both the patient and the provider. It’s a rigorous process, but it’s the right thing to do for better quality medicine.”
What’s Next for PCMH?
A new set of standards will be coming out in 2017 and are expected to be released this fall. 7 NCQA is working towards offering virtual reviews, said Proctor. “Going forward, the application process will take place by webinar where practice will show how they’re meeting certain requirements using their software. Right now, practices have to document how they’re meeting requirements with screenshots and other documentation, which can be very time-consuming,” he said. “This change will make the process considerably less intensive in terms of documentation.”
Practices can apply using the new standards starting March 31, 2017. “It is my recommendation that if practices don’t have any existing PCMH recognition and are considering getting recognition within the next year, they should use the 2014 standards and not wait to use the upcoming 2017 standards,” said Proctor. “While using 2014 standards will require more documentation, one benefit of using 2014 standards is that practices can attain recognition for a three-year period. With 2017 standards, recognition is only for one-year with annual reporting requirements in order to sustain recognition.”
“Meaningful Use nearing its end for Medicare practices may bring considerable changes to 2017 PCMH requirements as well. “Historically, Meaningful Use requirements have been fully embedded in PCMH standards, with NCQA continuing reporting requirements that have since been phased out of the Meaningful Use program,” said Proctor. “It will be interesting to see if NCQA updates its standards to remove some of the legacy Meaningful Use requirements.”
The application process can also be difficult to navigate. Practices that are getting ready to re-apply, like Hershey Pediatrics, are hoping NCQA will provide more clarity for 2017. “I would hope that the language they’re using is a little clearer so it’s easier for practices to understand what they’re looking for,” said Spangler. “The way NCQA worded questions made it hard to decipher what they were looking for. We would have been totally lost if we hadn’t hired a consultant to help us navigate the process.”
Should My Practice Apply?
While Dr. Rogu echoed Spangler’s sentiments that the process become less cumbersome, he also said he thinks PCMH recognition should become a requirement for pediatric practices. “The Patient-Centered Medical Home concept was invented by pediatricians. It’s ingrained in the way we practice medicine,” he said. “It’s becoming the norm. I think practices that don’t become PCMH recognized will eventually be excluded by the insurance carriers.”
Proctor offers some additional guidance for practices. “I usually get the question: ‘I heard about this Medical Home thing, but I don’t know if I should do it or not.’ I always tell people to start by checking to see if the payers they work with offer incentives, or if there are locally funded resources to help you through the transformation process. The process is time-consuming and expensive because there’s so much overhead involved. You often need to have someone working on this full-time to get your practice organized and gather documentation.”
“I encourage everyone to talk with other practices who have gone through the process and to work with your EHR vendor or consultant to see how you could better utilize software to meet PCMH requirements,” said Proctor. “In the end, getting PCMH recognition will allow you to stay competitive while improving patient care and operations.”
[1] “The Patient-Centered Medical Home: History, Seven Core Features, Evidence and Transformational Change,” Robert Graham Center for Policy Studies in Family Medicine and Primary Care, last modified November 2017, https://www.aafp.org/dam/AAFP/documents/about_us/initiatives/PCMH.pdf ↑
[2] “Considering PCMH: 8 Things You Should Know,” Physician’s Computer Company, last modified December 29, 2015, https://blog.pcc.com/considering-pediatric-pcmh-8-things-you-should-know ↑
[3] “Patient-Centered Medical Home,” National Committee for Quality Assurance, https://www.ncqa.org/programs/health-care-providers-practices/patient-centered-medical-home-pcmh/ ↑
[4] “Patient-Centered Medical Home,” National Committee for Quality Assurance, https://www.ncqa.org/programs/health-care-providers-practices/patient-centered-medical-home-pcmh/#sthash.ervnPbHB.pdf ↑
[5] “Your Own QI Project,” American Board of Pediatrics, https://www.abp.org/content/your-own-qi-project ↑
[6] “PCMH & PCSP Recognition Program Pricing,” National Committee for Quality Assurance, http://www.ncqa.org/programs/recognition/ncqa-pcmh-pcsp-recognition-program-pricing ↑
[7] “Recognition Redesign: Frequently Asked Questions,” National Committee for Quality Assurance, http://www.ncqa.org/programs/recognition/practices/patient-centered-medical-home-pcmh/pcmh-redesign/faq ↑
Katy Demong has a B.A. in English writing from St. Lawrence University and an MFA in writing from Goddard College. She’s been writing about current issues in health care and health information technology for almost 10 years. She lives in Salt Lake City, Utah and loves playing tennis and hiking with her dog.